July marks National Minority Mental Health Awareness Month, a crucial time to address mental challenges among people of color. In this first article, Impireum will mainly discuss the various behavioral health issues that U.S. BIPOC (Black and Indigenous People of Color) adults and seniors are currently facing.
Later in the month, we’ll address mental health awareness topics concerning BIPOC youth and young adults. Understanding this unique population’s mental health landscape is essential for fostering awareness and encouraging positive change.
Mental wellness issues disproportionately affect people of color in the U.S. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), in 2021, approximately 19.2% of Black adults and 17.3% of Hispanic adults experienced mental illness, compared to 22.6% of white adults.
However, these figures often underestimate the actual prevalence due to under-reporting and lack of access to mental health care. Among elderly1 populations, people of color are particularly vulnerable, with higher rates of depression and anxiety reported but significantly lower rates of treatment and diagnosis.
The COVID-19 pandemic exacerbated mental health issues across all demographics, with people of color being among the hardest hit. Studies show a significant increase in depression and anxiety rates starting in 2022, with minority communities experiencing heightened trauma and stress due to economic instability, health disparities, and loss of loved ones.
The American Psychological Association (APA) reported that Black and Hispanic adults, especially women2, were more likely to report symptoms of anxiety and depression than their white counterparts during and after the pandemic.
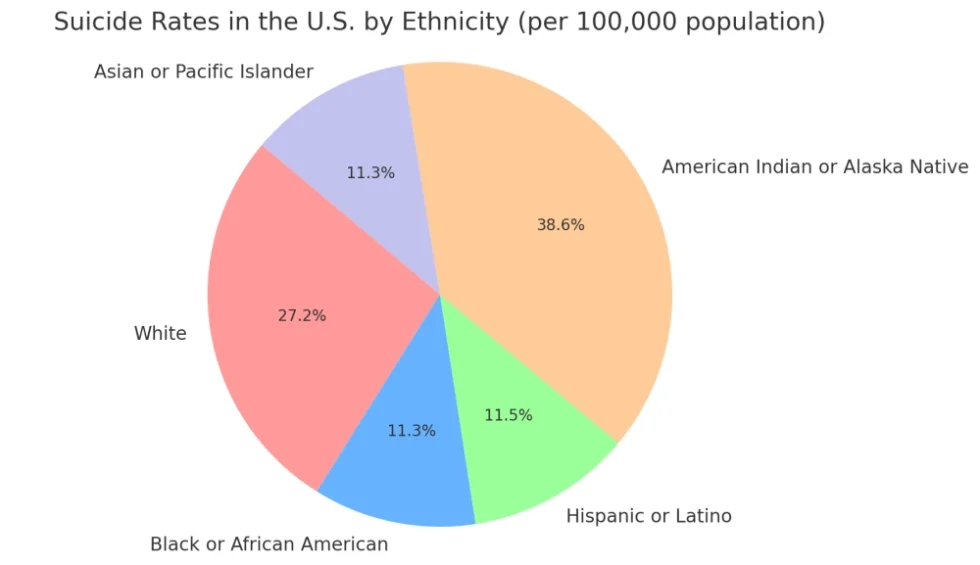
As of the most recent 2021 data, the annual suicide rates among the BIPOC population in the U.S. remain lower compared to whites, with one exception. However, there are critical nuances worth noting:
According to the Centers for Disease Control and Prevention (CDC)3, the suicide rate among Black Americans is approximately 7.4 per 100,000 as of 2021. This number is significantly lower than the rate for white individuals, which is roughly 18.3 per 100,000.
The suicide rate among Hispanic individuals is about 7.8 per 100,000. This rate is also lower than that of white individuals but has been increased in recent years.
This group has a lower overall suicide rate, at around 6.6 per 100,000. However, disparities exist within subgroups, with some experiencing higher rates of suicide. Underreporting is the most significant variable that could pose an annual threat to the results of actual reported percentage rates.
Unfortunately, this group still faces the highest suicide rates among all racial/ethnic groups, at approximately 23.9 per 100,000. This rate is significantly higher than that of white individuals and highlights severe mental wellness disparities within this community.
In all, the reported suicide rates for Black, Hispanic, and Asian American populations are lower compared to white individuals, while rates among American Indian or Alaska Natives remain highest. Yet, the increasing trends and unique challenges faced by these communities still underscore the need for targeted mental health interventions and support.
NATIONAL SUICIDE LIFELINE— Dial or Text 988 for immediate assistance!
Barriers to mental health care among minority populations include socioeconomic challenges, lack of insurance, and cultural mistrust of healthcare systems.
People of color often face treatment disparities, with fewer options for culturally competent care and lower rates of follow-up treatment. The National Alliance on Mental Illness (NAMI) highlights that only one in three Black adults with mental health issues receives treatment, compared to nearly half of white adults.
Stigma and societal pressures still significantly deter people of color from seeking mental health services. Cultural stigmas surrounding mental health often label those seeking help as weak, leading to internalized shame and reluctance to access care. Societal pressures, including discrimination and racial trauma, also contribute to the mental health burden, creating a vicious cycle of untreated mental illness.
In addition, programs aimed at training more culturally competent mental health professionals are also expanding.
Community health centers and telehealth/telepsychiatry services have also become valuable resources, providing more accessible and flexible treatment options. In addition, there are initiatives like the APA’s Minority Fellowship Program. This program aims to increase the number of minority mental health professionals, enhancing the diversity and cultural competence within the field.